Eliminating Communication Breakdowns in Post-Acute Care with NLP AI Technologies
In late March, a patient with metastatic cancer arrived at a skilled nursing facility, where she, unfortunately, was supposed to be admitted into hospice care. However, the paper-based packet of discharge orders that accompanied her transfer didn’t contain the instructions for hospice care or pain relief. And because this breakdown in information transfer occurred on a Friday afternoon, the facility was unable to make the right arrangements until the weekend was over.
“I can’t give them the help that they need because [the industry operates] with paper and envelopes that are hand-delivered, and when I ask for a copy of that discharge packet, no one knows how to get it to me,” patient advocate Grace Cordovano shared in an emotional LinkedIn post. “We need a hospice order now, but everything’s closed. It’s just not fair. And it shouldn’t be this hard, not when you’re dying of cancer.” This patient had to needlessly suffer in pain all weekend.
This is an example of what can go wrong when care information isn’t available in an easily digestible form at the point of admission. And, as the 128 comments on Grace’s post show, it’s a situation that is altogether too common, no matter the day of the week.
For these organizations, integrating a data exchange platform with innovative solutions like Natural Language Processing (NLP) and Artificial Intelligence (AI) offers a practical way to speed information transfer and make data actionable for staff and clinicians to support better care.
Vital Elements of a Post-Acute Care Toolkit
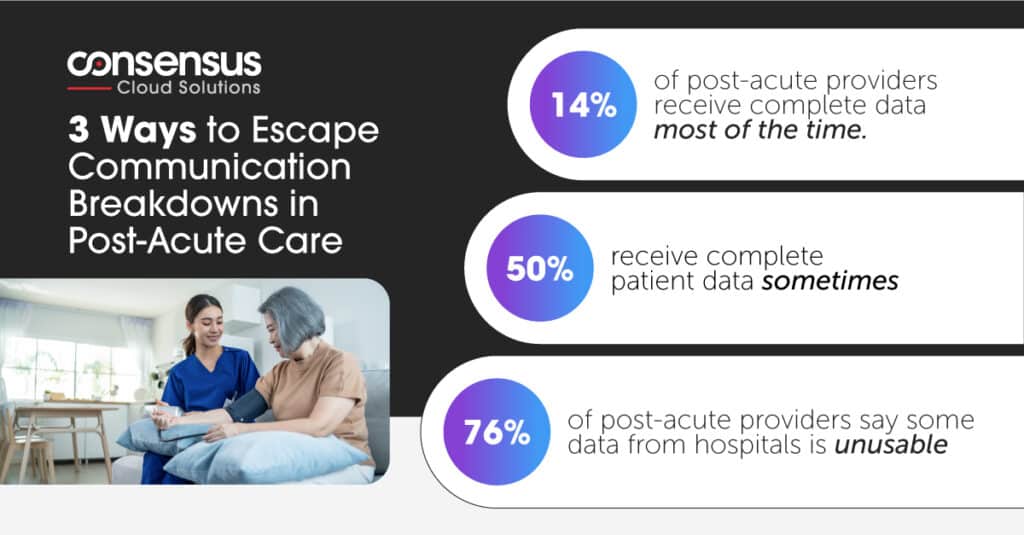
As the linked, real life experience demonstrates, breakdowns in information transfer can have heartbreaking consequences for post-acute care patients and their families. Yet most skilled nursing facilities (SNFs) and post-acute care facilities lack meaningful connectivity with their referral partners. More than half say they sometimes or often receive patient information after the patient is in their care. Even when the information does arrive, 76% report that at least a portion of the data isn’t usable or it’s incomplete. This not only slows down admission processes, but it also prevents patients from receiving critically needed care.
This isn’t just an issue of post-acute facilities not having EHR funding. While it would be great for healthcare organizations to all be on one system, the reality is that even within a single organization, most providers work from disparate systems. Organizations like Kaiser—where every hospital, ambulatory facility, physician practice and even the health plan is on Epic—are the exception rather than the rule.
Without the technology to put data at clinicians’ fingertips, continuity of care will suffer. It’s an area where NLP and AI technologies can make a substantial difference when implemented as part of the data workflow.
Staffing shortages alone make it imperative that team members can quickly translate the information on intake forms into next steps for care. When applying NLP with AI, a digital cloud fax can be transformed into structured data, even if the content is in handwriting. When that data can be mapped to specific fields on the receiving side using a powerful integration engine, it can be transmitted automatically without the need for human data entry. This makes it easy for the data to be shared with clinicians directly within their workflows, in a format with which they are highly familiar. It also empowers team members to determine, at a glance, why the post-acute transfer was initiated and the types of support the patient requires.
Data that is extracted from an unstructured document can be sent as a DSM, HL7 or FHIR message—much like a secure email—to a clinician, physician or provider. NLP and AI capabilities can be integrated with other solutions—like electronic signature tools, robotic process automation, and integration platforms—to streamline communication and data sharing across multiple care settings.
A High-Value Approach for Better Transitions in Care
At a time when skilled nursing facilities, critical access hospitals, and care settings in under-served areas are still recovering from the financial and operational stresses of the pandemic, NLP AI solutions like Consensus’ Clarity, combined with integration solutions like Consensus’ Conductor, offer all providers a sophisticated-yet-affordable solution for better continuity in post-acute care at an attainable investment point. These technologies provide a transformative, yet practical, approach to ensure that post-acute care clinicians receive the right information directly within their workflows, which enables them to provide the right patient care as quickly as possible. More importantly: They help avoid needless suffering and heartbreaking scenarios that leave patients, families, and clinicians feeling powerless.
Click here to learn about the 3 Ways to Escape Communication Breakdowns in Post-Acute Care.
Read more about Consensus’ approach to NLP and AI in healthcare. Want to continue the conversation? Please reach out.